If you have ever experienced the discomfort of temporomandibular joint dysfunction (TMJ), then you know firsthand how much the pain can affect your daily activities. Using a TENS unit can help and knowing where to place the electrode pads is very important.
TENS Placement for TMJ
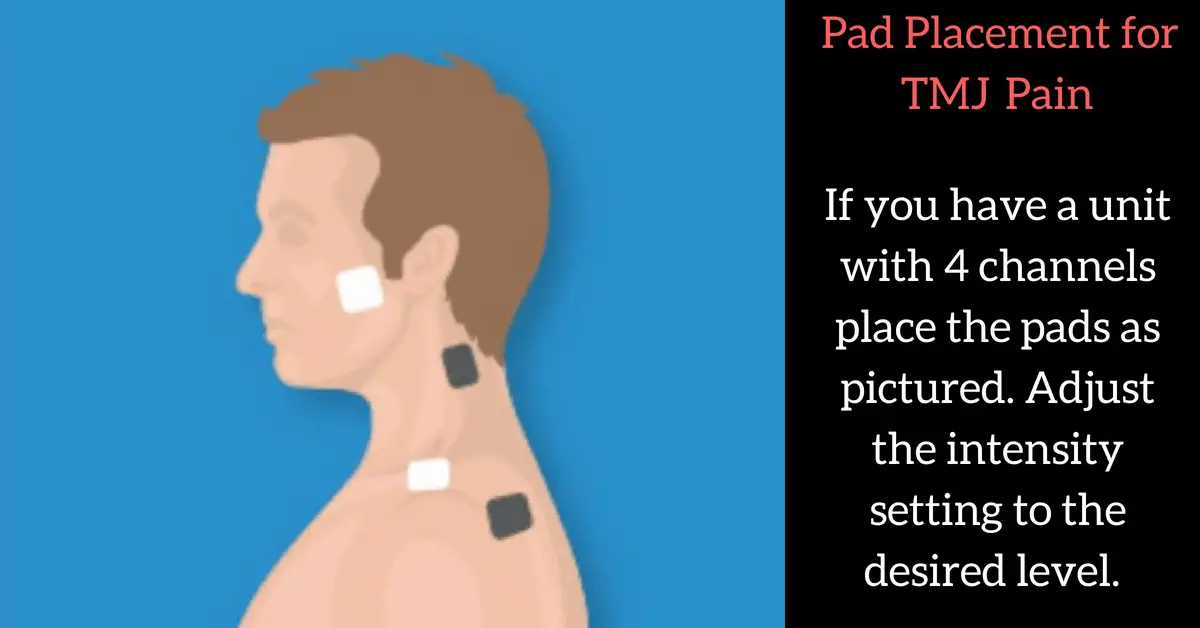
Usually the TENS electrode pads are placed on each temporomandibular joint, as well as at the neck below the base of the head. This placement can help relieve several of the symptoms that come with TMJ such as headaches, neck pain, and back pain.
TENS unit electrode placement for TMJ is not an exact science and is different for everyone depending on their individual symptoms.
If you’re considering using a TENS unit placement for TMJ other than this, you should first consult with your physician.
When using your TENS unit to treat pain for TMJ always start off on the lowest intensity level for starters. The preferred setting will feel like a gentle to moderate tingling feeling. If you feel a strong twictch in your facial muscles turn down the intensity level.
How High Should I Set My TENS Unit? click here to read what settings to use.
Best TENS unit for TMJ Pain
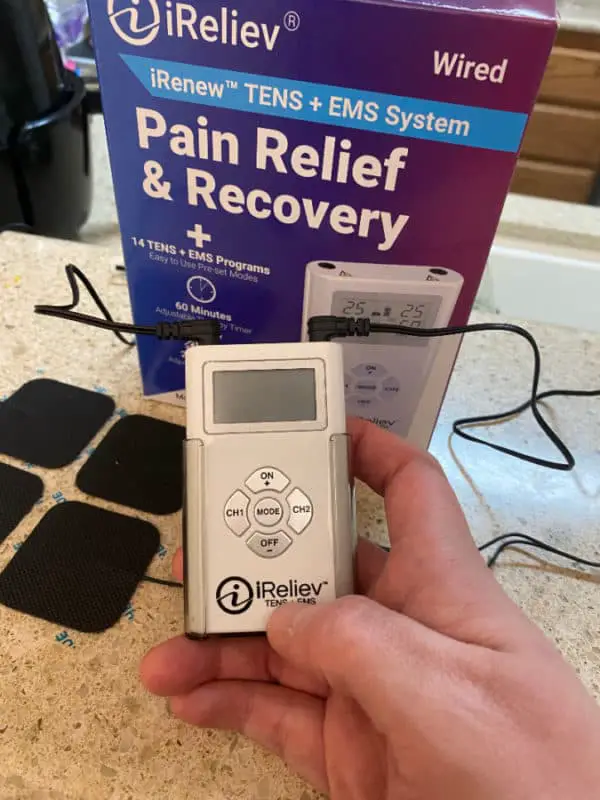
This is the exact TENS unit that I use. It is perfect for treating TMJ. The iReliev is a great little device and has a lot of going for it. It is under $80 and has several programs to choose from and is small enough to fit in your pocket.
You do not need to spend hundreds of dollars to get a quality TENS unit and iReliev gives you a ton of value for the price being paid. Best part is they are based in Dallas, Texas and have phenomenal customer service.
Get yours today on the iReliev website by clicking here.
Want to know where else a TENS unit can be placed? Check out my TENS placement guide for how to use one for-
Knee Pain
Neck Pain
Shoulder Pain
Tension Headaches
Golfer’s Elbow
Plantar Fasciitis
Rotator Cuff Pain
Restless Leg Syndrome
Check out this testimonial video from a patient who finally found relief from her TMJ symptoms by using a TENS unit:
We don’t know exactly what causes TMJ, but doctors believe symptoms are caused from problems with the muscles of your jaw or with the parts of the joint itself. Injury to your jaw, the joint, or the muscles of your head and neck can lead to TMJ.
Other causes include grinding or clenching your teeth, which puts a lot of pressure on the joint, movement of the soft cushion or disc between the ball and socket of the joint, arthritis in the joint, and stress, which can cause you to tighten facial and jaw muscles or clench the teeth.
The symptoms of TMD are widely varied and can include pain or tenderness in your face, jaw joint, neck and shoulders, and ear when you chew, speak, or open your mouth wide, jaws that get “stuck” or “locked” in the open- or closed-mouth position, clicking, popping, or grating sounds in the jaw joint when you open or close your mouth or chew.
You may also experience pain, a tired feeling in your face, trouble chewing or a sudden uncomfortable bite — as if the upper and lower teeth are not fitting together properly or swelling on the side of your face.
You may also have toothaches, headaches, neck aches, dizziness, earaches, hearing problems, upper shoulder pain, and ringing in the ears (tinnitus).
When you open and close your mouth, many muscles, ligaments, and joint structures have to all work in perfect unison to create a smooth and pain-free movement. Researchers are just now starting to understand exactly how it functions and the best ways to treat pain coming from the area.
TMD is a cluster of related disorders in the masticatory system that has many signs and symptoms such as:
- tenderness in the muscle and joint
- decreased range of motion
- clicking, stiffness
- pain or fatigue in facial muscles
- ear symptoms like tinnitus, fullness
- vertigo
- sensation of variable bite changes
- deviation to the affected site during opening
- jaw catching during opening or closing
These symptoms can make it painful and uncomfortable to eat, speak, drink, smile, and sleep normally.
For most people, TMJ issues will resolve after a short period of time without any treatment.
Unfortunately, some people will also develop chronic or recurring pain associated with the joint that requires some type of treatment.
Usually a combination of dental appliances, exercises, and lifestyle changes will create significant relief for these people. There are many different types of treatment for TMJ problems, and most people will need to use several different techniques to gain long term relief.
The first thing to understand with TMJ treatment is that you should attempt every type of treatment that is available before doing anything that will cause permanent changes.
Except in some very limited situations, surgery or permanent treatments generally aren’t recommended by the most current expert recommendations. Surgery is rarely done for people with TMJ issues, and generally the only people who need surgery are those whose joints have physically deteriorated.
This is always the last option to consider since there is usually a significant recovery involved and the results are not guaranteed to be consistent.
You generally can’t make the problem any worse than it already is by relying on non-surgical treatments. The permanent treatments on the other hand can potentially cause long term damage and sometimes make the problem worse.
It is also important to remember that the types of treatment you seek out also depend on what kind of TMJ issue it is. Suggestions that are helpful for most people with TMJ problems are dental appliances, hot compresses, and exercises.
There are things you can do on your own to help relieve TMD symptoms.
Your doctor may suggest you take over-the-counter medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), like naproxen or ibuprofen, can relieve muscle pain and swelling.
Your dentist can prescribe higher doses of NSAIDs if you need them for pain and swelling. He might suggest a muscle relaxer to relax your jaw if you grind or clench your teeth. Or an anti-anxiety medication to relieve stress, which may bring on TMD. In low doses they can also help reduce or control pain.
Muscle relaxants, anti-anxiety drugs, and antidepressants are available by prescription only.
Applying a moist heat or cold pack to the side of your face and temple for about ten minutes may also relieve TMD discomfort.
If your doctor or dentist approves, my can also do a few simple jaw stretches. When you’re done, hold a warm towel or washcloth to the side of your face for about 5 minutes, and perform this routine a few times each day.
Try to eat soft foods and avoid extreme jaw movements to keep TMD symptoms from worsening.
Keep yawning and chewing to a minimum and don’t yell, sing, or do anything that forces you to open wide. Also, try to keep your teeth slightly apart as often as you can. This will relieve pressure on your jaw. Put your tongue between your teeth to control clenching or grinding during the day.
Learning relaxation techniques can also help loosen up your jaw. Ask your doctor if you could benefit from physical therapy or massage. Your dentist could also recommend a splint or night guard. These plastic mouthpieces fit over your upper and lower teeth so they don’t touch.
They lessen the effects of clenching or grinding and correct your bite by putting your teeth in the correct position. The difference between the mouthpieces is that you wear night guards while you sleep, and you use a splint all the time.
Your dentist can also replace missing teeth and use crowns, bridges, or braces to balance the biting surfaces of your teeth or to correct a bite problem.
There is also limited evidence that certain types of chiropractic care can help with TMJ dysfunction. Chiropractic treatment can be similar to physical therapy or massage of the area.
Exercises for TMJ
Isometric exercises for TMJ can also be performed by applying a counter-resistant force to the movement being performed.
Forcefully placing the chin on a closed hand during depression jaw movement (mouth opening) and hindering its elevation (closing) by pressing the inferior incisors with the index and middle fingers are considered muscular strengthening exercises that depress and elevate the jaw, respectively.
In lateral jaw movements, the counter-resistance force is applied by pressing the lateral area of the jaw with the index and middle fingers, exerting a force opposite to the movement performed. These exercises should be repeated several times a day under the guidance of a medical professional.
A TENS unit is a device that sends small electrical currents to targeted body parts to relieve pain. Some TENS units are designed for use in a hospital or healthcare facility and others are safe to use at home.
A TENS unit sends electrical pulses through the skin through carefully placed electrodes which control pain signals in the body, creating temporary or permanent relief from pain associated with arthritis, surgery, bursitis, migraines, and injuries.
Some people experience permanent pain relief after repeated sessions with a TENS unit and others need TENS therapy for a prolonged period. The effectiveness ranges by condition and intensity of treatment.
The frequency of the currents coming from a TENS unit can be turned up or down, ranging from about 10 Hz to 50 Hz. The pulse delivered by the TENS unit only penetrates the skin to the level of the nerve fibers, less than one inch, which poses no danger to most patients.
Electric nerve stimulation is generally regarded as safe, but it can have risks just like any other medical procedure.
For example, if the electrical current is too high or the electrodes are placed on the wrong part of the body, this can burn or irritate the skin. The “danger zones” include the brain, heart, eyes, and throat.
People with epilepsy, heart problems, pregnancy, or implanted devices, including infusion pumps, pacemakers, and defibrillators, should not use TENS treatment.
There has been a limited amount of research done on the use of TENS therapy for TMJ pain reduction and improved jaw movement
Several studies have shown encouraging results. Pain associated with TMJ is typically the result of muscle strain and nerve pressure.
When your jaw muscles are combating the hard tissues of your jaw and skull, they not only strain themselves and put pressure on local nerves, but pull other muscles out of alignment, which creates a cascade effect as those muscles put pressure on other nerves.
The first way to relieve the pain associated with TMJ is to get your muscles to relax. TENS does this through its auto-massage.
The TENS units used in dentistry are different from those used in chiropractic and other applications, where the goal is to block pain signals–dental TENS units actually work to relieve the root cause of pain and provide a good starting place for long-term treatment.
Active TENS therapy showed favorable results in pain management in TMD patients, especially in muscular or chronic pain and mouth opening, as compared to the placebo TENS therapy.
The success rate of TENS therapy for the treatment of TMD could be as high as 75% but this number widely varies between studies.
The difference in the success rates could be due to the disparity between the study samples regarding differences in biological, psychological, and social components affecting the TMDs, as well as the stimulation parameters used in the TENS therapy.
Most studies reveal that it takes about 30 minutes for low-frequency TENS treatment to begin alleviating pain. Some patients report feeling hours of pain relief from 30-to-60-minute sessions.
Thank you for reading,
References
https://www.healthline.com/health/transcutaneous-electrical-nerve-stimulation-unit
http://www.imedpub.com/articles/pain-management-in-temporomandibularjoint-disorders-by-active-and-placebotranscutaneous-electric-nerve-stimulationa-comparative-st.pdf
https://www.webmd.com/oral-health/guide/temporomandibular-disorders-tmd#1-2